As a rheumatologist, one of the most common concerns I address is bone health. Osteoporosis and osteomalacia, while both conditions that affect the bones, have different causes, symptoms, and treatment approaches. It’s crucial for patients, particularly those at risk, to understand these differences in order to seek the appropriate care and prevent complications.
Osteoporosis: When Bones Become Brittle
Osteoporosis is a condition where bones lose density and become fragile. It’s often referred to as the “silent disease” because it progresses without any noticeable symptoms until a fracture occurs. Most commonly affecting postmenopausal women and older adults, osteoporosis is linked to hormonal changes, lack of physical activity, and insufficient intake of calcium and vitamin D.
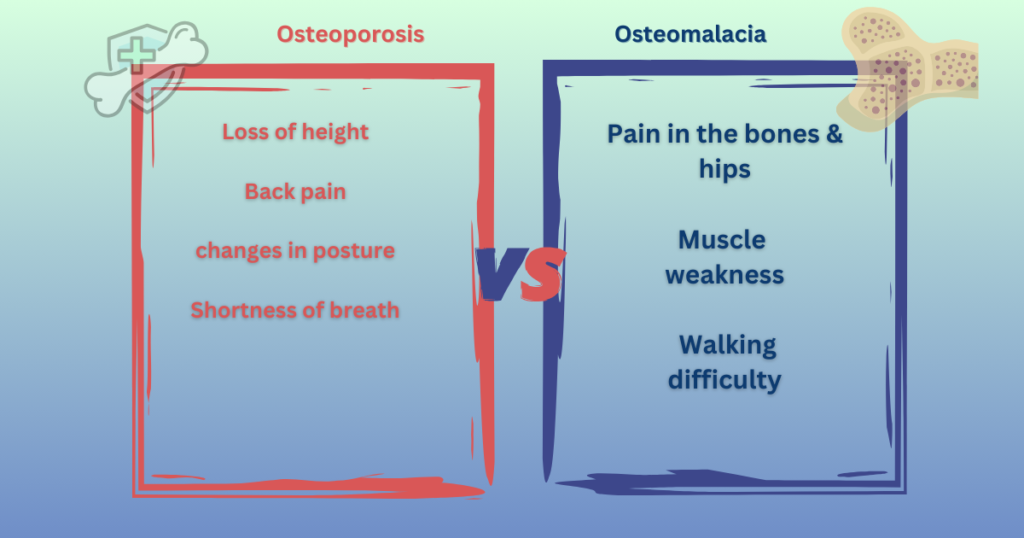
Symptoms:
- Unexplained fractures, especially in the spine, hips, or wrists
- Loss of height over time
- Back pain due to compressed vertebrae
Management: It can be managed through early detection with bone density testing (DEXA scan), adequate calcium and vitamin D intake, weight-bearing exercises, and medications like bisphosphonates or selective estrogen receptor modulators (SERMs).
Osteomalacia : Softening of the Bones
Unlike osteoporosis, osteomalacia results from a deficiency in vitamin D, which is crucial for the body to absorb calcium. When vitamin D levels are too low, the bone mineralization process is impaired, causing the bones to soften. This leads to bone pain, muscle weakness, and an increased risk of fractures.
Symptoms:
- Pain in the hips, lower back, and legs
- Muscle weakness and difficulty walking
- Increased risk of bone deformities
Management: Treatment involves correcting vitamin D deficiency through supplements and increased sun exposure. Calcium intake is also important to support bone mineralization. In cases where absorption is an issue, additional measures may be required.
Why Understanding the Difference Matters
As a healthcare provider, I strongly recommend that patients, particularly those at higher risk of bone-related issues, undergo regular screening. Early detection through bone density testing can help manage osteoporosis before fractures occur. On the other hand, osteomalacia can often be corrected with proper vitamin D supplementation, making early diagnosis key.
For those with osteoporosis, maintaining bone density through medication and lifestyle changes like regular physical activity can prevent fractures and enhance quality of life. For osteomalacia, a combination of dietary adjustments, supplementation, and increased sunlight exposure can restore bone health.
FAQ:
1. What are the key differences between osteoporosis and osteomalacia?
Osteoporosis is characterized by decreased bone density, making bones fragile and prone to fractures, while osteomalacia involves softening of the bones due to a deficiency in vitamin D and impaired bone mineralization.
2. How are osteoporosis and osteomalacia diagnosed?
Osteoporosis is commonly diagnosed through a bone density test (DEXA scan), while osteomalacia is typically identified through blood tests to check for vitamin D deficiency, along with imaging and sometimes bone biopsy.
3. Can osteoporosis and osteomalacia be treated?
Yes, both conditions are treatable. Osteoporosis treatment focuses on medications to strengthen bones, along with calcium and vitamin D supplements. This treatment primarily involves vitamin D supplementation and calcium intake.
4. Is vitamin D deficiency the only cause of osteomalacia?
No, while vitamin D deficiency is the most common cause, it can also result from certain medical conditions such as kidney disorders, malabsorption syndromes, or the use of certain medications.
5.Where can I seek treatment for osteomalacia in Ahmedabad?
Dr. Dhaiwat Shukla provides expert care for osteomalacia and other bone health concerns at specialized facilities in Ahmedabad. Services include vitamin D assessments, tailored supplementation plans, and comprehensive management.
Conclusion: Protect Your Bone Health
Both osteoporosis and osteomalacia can significantly impact your bone health if left unaddressed. By understanding the differences between the two conditions, you can take proactive steps to protect your bones and prevent further damage. If you’re experiencing symptoms or are at risk, it’s essential to consult with a rheumatologist to discuss diagnosis and treatment options tailored to your needs.
Your bone health matters, and with the right approach, you can manage and even prevent these conditions from affecting your quality of life.